We have been coordinating with the Department of Health Care Services (DHCS) in an effort to share all new ALW/Medi-Cal updates with you all. We recently became aware of the tier change approvals and some potential ALW billing issues that you all may be facing (or may soon face), so we are including some information below for you all so as to clarify any of those potential issues since DHCS is incredibly backlogged and trying to catch up on all processing.
Communities do still have to wait until the tier change approval to begin billing at the higher rate and to back-bill the difference.
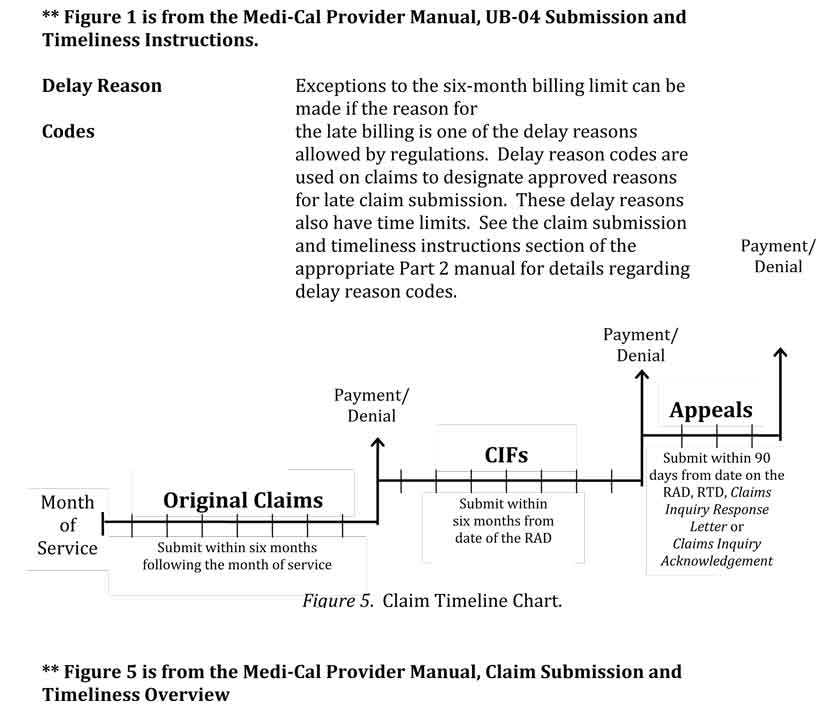
- There may be some issues with timing since Medi-Cal requires providers to bill within 6 months of the original service date or they may ultimately deny the claim for back pay, or may only pay a portion of the back pay.
- In order to avoid this, the community will need to include a delay reason code when submitting for a reimbursement once the tier change approvals come through, in order to avoid a denial code or reduced payment.
Below is some information that is included in the Medi-Cal Provider Manual and may be useful information for you to keep on hand.
| Cause of Delay | Delay Reason Code | Documentation Needed |
| Retroactive SSI/SSP | 10 | Copy of the original County Letter of Authorization (LOA) form (MC-180) signed by an official of the county. |
| Court order | 10 | Same as previous |
| State or administrative hearing | 10 | Same as previous |
| County error | 10 | Same as previous |
| Department of Health Care Services (DHCS) approval | 10 | Same as previous |
| Reversal of decision on appealed Treatment Authorization Request (TAR) | 10 | Copy of the TAR, copy of the DHCS letter or court order reversing the TAR denial, and an explanation of the circumstances in the Remarks field (Box 80) of the claim. |
| Medicare/Other Health Coverage | 10 | Copy of the Other Health Coverage Explanation of Benefits and an explanation of the circumstances in the Remarks field (Box 80) of the claim. |
Figure 1. Over-One-Year Billing Exceptions.